The Centers for Medicare & Medicaid (CMS) announced in the fiscal year 2022 Hospital Prospective Payment System final rule published on August 2,2021 that it was adopting an April 1 implementation date for ICD-10-CM and ICD-10-PCS code updates, in addition to the annual October 1 update, beginning with April 1, 2022. The April 1 implementation used a phased-in approach, such that the number and nature of code updates were fewer and less comprehensive as compared to the existing October 1 update. The intent of the April 1 implementation date was to allow flexibility in the ICD-10-CM/PCS code update process. CMS believes that this additional April 1 implementation date for new codes allows for “earlier recognition of diagnoses, conditions, and illnesses as well as procedures, services, and treatments in the claims data. The agency also believes this earlier recognition would be beneficial for purposes of reporting data collection, tracking clinical outcomes, claims processing, surveillance, research, policy decisions, and data operability. “1
1 AHIAMA Journal September, 20 2021 Highlights of FY2022 IPPS Final Rule
Guidelines for Achieving a Compliant Query Practice (2022 Update)
The 2022 Updated Guideline for Achieving a Compliant Query Practice was approved and its final version was published December 2022.
“The documentation query process is used for several initiatives which may include reimbursement methodologies, data stewardship and collection, quality measures, medical necessity, denial prevention, and so forth. Regardless of organizational objectives, professionals seeking documentation clarification need to follow this practice brief.”1
As sepsis is one of the top diagnosis if not the top diagnosis in the nation to be denied by payors with, severe malnutrition, metabolic encephalopathy and respiratory failure not far behind, it is more important than ever to make sure the documentation in the patient record is sufficient to support the assignment of these diagnoses and others.
Queries should be accompanied by the relevant clinical indicators that show why a more complete or accurate diagnosis or procedure is requested.
“Clinical indicator(s)” is a broad term encompassing documentation that supports a diagnosis as reportable and/or establishes the presence of a condition. Two Examples of clinical indicators include (but are not limited to): provider observations (physical exam and assessment), diagnostic tests, treatments, medications, trends, and consultant documentation authored by providers and ancillary professionals documented throughout the health record. There is no required number of clinical indicator(s) that must accompany a query because what is a “relevant” clinical indicator will vary by diagnosis, patient, and clinical scenario.2
It is ultimately up to the providers to make the final determination as to what clinical indicator(s) define a diagnosis.
Clinical indicators should:
- Be clear and concise
- Directly support the condition requiring clarification
- Allow the provider to clinically determine the most appropriate medical condition or procedure
- Paint the clinical picture of the diagnosis queried to be added or clinically validated
- Be specific or directly related to, but not necessarily from, the current encounter (Read new Query Brief as to Role of Prior Encounters in Queries) Support documentation that will translate to the most accurate code
Clinical indicator(s) may be sourced from the entirety of the patient’s health record, including but not limited to:
- Emergency services documentation (e.g., emergency service transport, ED provider, ED nursing)
- Diagnostic findings (e.g., laboratory, imaging)
- Provider impressions (e.g. history and physical, progress notes, consultations)
- Relevant prior visits (if the documentation is clinically pertinent to present encounter)
- Ancillary professional documentation and assessments (e.g., nursing, nutritionist, wound care, physical, occupational, speech, and respiratory therapist)
- Procedure/operative notes
- Care management/social services
1. Guidelines for Achieving a Compliant Query Practice (2022 Update)
2. Compliant CDI Technology Standards (2021). AHIMA/ACDIS. Retrieved from: Compliant CDI Technology Standards
New & Updated General Coding Guidelines (2022 – 2023)
In this section:
- Laterality
- Documentation by Clinicians Other than the Patient’s Provider
- Documentation of Complications of Care
- History of HIV Managed by Medication
- Use of Z Codes
Disclaimer:
The information presented here is not intended to serve as coding or legal advice. Many variables affect code selection and sequencing. All coding must be considered on a case-by-case basis as supported by the documentation in the medical record.
Payer-specific rules and regulations must also be taken into consideration in code selection. The information contained in this handout was accurate on the date of publication and is subject to change based on quarterly Coding Clinic updates from the American Hospital Association and yearly coding changes as determined by the National Center for Health Statistics and Centers for Medicare and Medicaid Services with approval from the World Health Organization.
Laterality:
When laterality is not documented by the patient’s provider, code assignment for the affected side may be based on medical record documentation from other clinicians. If there is conflicting medical record documentation regarding the affected side, the patient’s attending provider should be queried for clarification. Codes for “unspecified” side should rarely be used, such as when the documentation in the record is insufficient to determine the affected side and it is not possible to obtain clarification.
Documentation by Clinicians Other than the Patient’s Provider:
Code assignment is based on documentation by the patient’s provider. There are a few exceptions when code assignment may be based on medical record documentation from clinicians who are not the patient’s provider (i.e., physician or other qualified healthcare practitioner legally accountable for establishing the patient’s diagnosis).
These exceptions include codes for:
- Body Mass (BMI)
- Depth of non-pressure chronic ulcers
- Pressure ulcer stage
- Coma scale
- NIH stroke scale (NIHSS)
- Social determinants of health (SDOH)
- Laterality
- Blood alcohol level
- Underimmunization status
The BMI, coma scale, NIHSS, blood alcohol level codes, codes for social determinants of health and underimmunization status should only be reported as secondary diagnoses.
Documentation of Complications of Care:
There must be a cause-and-effect relationship between the care provided and the condition, and the documentation must support that the condition is significant. It is not necessary for the provider to explicitly document the term “complication.” For example, if the condition alters the course of the surgery as documented in the operative report, then it would be appropriate to report a complication code. Query the provider for clarification if the documentation is not clear as to the relationship between the condition and the care or procedure.
History of HIV Managed by Medication:
If a patient with documented history of HIV disease is currently managed on antiretroviral medications, assign code B20, Human immunodeficiency virus [HIV] disease. Code Z79.899, Other long term (current) drug therapy, may be assigned as an additional code to identify the long-term (current) use of antiretroviral medications.
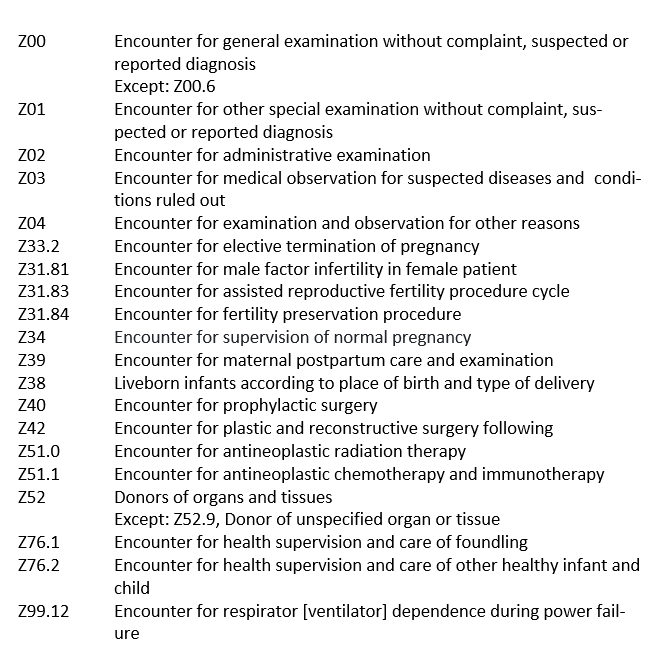
Use of Z Codes:
Z codes (other reasons for healthcare encounters) may be assigned as appropriate to further explain the reasons for presenting for healthcare services, including transfers between healthcare facilities, or provide additional information relevant to a patient encounter. The ICD-10-CM Official Guidelines for Coding and Reporting identify which codes maybe assigned as principal or first-listed diagnosis only, secondary diagnosis only, or principal/first-listed or secondary (depending on the circumstances).
Z Codes That May Only be Principal/First-Listed Diagnosis
ICD-10-CM Coding Tips
In this section:
- Rib Fracture due to Chest Compression
- New Codes for Nervous System Disorders
- Correctly Coding: Cerebrovascular Disease
- COVID Screening Update
- COVID-19 Exposure of Newborn
- Newborn Observation due to Maternal Marijuana Use
- Hyperlipidemia v. Hypercholesterolemia
- Kidney Transplant
- Anticoagulant
- Palliative Care
Rib Fracture Due to Chest Compression & Cardiopulmonary Resuscitation:
New subcategory M96.A
New subcategory M96.A, Fracture of ribs, sternum and thorax associated with compression of the chest and cardiopulmonary resuscitation has been created with new codes to specifically identify thoracic fractures due to performance of cardiopulmonary resuscitation (CPR) and chest compression.
Unfortunately, elderly patients and persons with pre-existing conditions are high risk for this type of injury. “When providing external chest pressure to support perfusion to the brain or other vital organs, rib fractures may be an unavoidable occurrence.”1
Note an external cause code from Chapter 20 is not assigned as an additional code because the external cause and intent are included in the subcategory codes for M96. A.
- M96.A1, Fracture of sternum associated with chest compression and cardiopulmonary resuscitation
- M96.A2, Fracture of one rib associated with chest compression and cardiopulmonary resuscitation
- M96.A3, Multiple fractures of ribs associated with chest compression and cardiopulmonary resuscitation
- M96.A4, Flail chest associated with chest compression and cardiopulmonary resuscitation
- M96.A9, Other fracture associated with chest compression and cardiopulmonary resuscitation.
***Note the above codes are complication/comorbid conditions
1 AHA coding Clinic Fourth Quarter 2022
New Cods for Nervous System Disorders:
As of October 1, 2023, coders can now report the following codes:
Postural orthostatic tachycardia syndrome (POTS) is a chronic autonomic nervous system disorder that can cause severe disability. “It can occur as a complication of another autoimmune or post-acute disorder.”1 Other terms used by physicians to document this disorder are chronic orthostatic intolerance or postural tachycardia syndrome. The ICD-10-CM code for this syndrome is G90.A.
Post-viral fatigue syndrome, G93.31, represents prolonged fatigue brought on by a virus such as the flu or COVID-19. “An ICD-10-CM code may not be reported based on documentation of fatigue due to COVID-19, as fatigue is a common symptom of many conditions and does not typically persist an extended period.”2 The documentation must specify “post-viral fatigue syndrome”.
There is now a new code for Myalgic encephalomyelitis/chronic fatigue syndrome G93.32. This syndrome is characterized by extreme fatigue with no exact cause known. There are more than 200,000 cases per year in US. This syndrome is more common in females.
1,2 – 2023 Neurology update: New ICD-10-CM codes for nervous system disorders
Correctly Coding: Cerebrovascular Disease:
Per AHA Coding Handbook it is appropriate to utilize reports to provide greater specificity of the anatomical site as documented by the provider. Coding professionals may need to review an X-ray report to identify the location of a fracture, or an imaging report, such as a magnetic resonance (MRI) study, to determine the location of the infarction or stroke in a patient diagnosed with a cerebral infarction or hemorrhagic stroke.
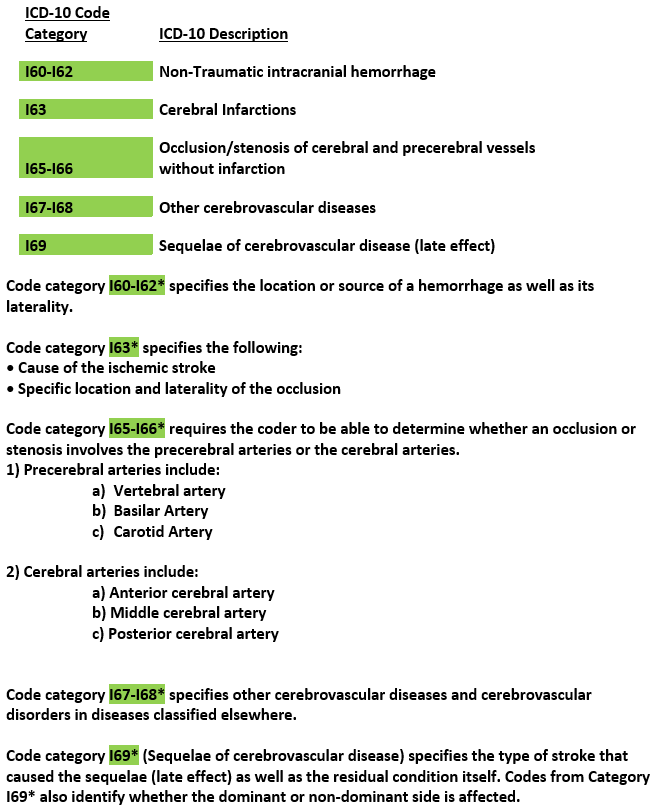
Coding guidelines state that the late effects (sequelae) caused by a stroke may be present from the onset of a stroke or arise at ANY time after the onset of the stroke.
Note: If a patient is NOT EXPERIENCING A CURRENT CEREBROVASCULAR ACCIDENT (CVA) and has no residual or late effect from a previous CVA, Z86.73 (personal history of transient ischemic attack, and cerebral infarction without residual deficits) should be assigned. A patient experiencing no residual effects from a previous stroke should NEVER be assigned a current stroke code.
In order to accurately code sequelae (late effect) of cerebrovascular disease, the side of the body affected should be clearly documented in the medical record.
COVID Screening Update:
Beginning October 1, 2023, (due to the fact that the COVID-19 Public Health Emergency ended on May 11, 2023), the “FY24 ICD-10-CM Official Guidelines for Coding and Reporting” have been revised to state that code Z11.52, Encounter for screening for COVID-19, should be assigned for encounters for screening for COVID-19 infection.”1 During the COVID-19 pandemic, a screening code was generally not appropriate for encounters for COVID-19 testing, including preoperative testing, and coders were directed to code as exposure to COVID-19, Z20.822, Contact with and (suspected) exposure to COVID-19 (guideline I.C.1.g.1.e).
1 AHA Coding Clinic, Volume 10 First Quarter, Number 1, 2023
COVID Exposure of Newborn:
Per Coding Clinic Second Quarter 2022 the question was asked whether to assign the code Z20.822, Contact with and (suspected) exposure to COVID-19 on a healthy newborn record when the infant’s mother had been diagnosed with COVID-19 during her second trimester of pregnancy. Coding Clinic advised to not assign the code Z20.822 since the provider’s documentation did not indicate the infant had been affected by the mother’s COVID-19 infection and the criteria for secondary diagnosis had not been met.
The Official Guidelines for Coding and Reporting general perinatal rules (16. a.6.) state “All clinically significant conditions noted on routine newborn examination should be coded. A condition is clinically significant if it requires: clinical evaluation, or therapeutic treatment, or diagnostic procedures, or extended length of hospital stay, or increased nursing care and/or monitoring, or has implications for future health care needs.”
Newborn Observation due to Maternal Marijuana Use:
The following question was asked in Coding Clinic First Quarter 2022.
Question: How is the diagnosis of intrauterine drug exposure correctly reported on a newborn’s record? In the example given an infant was born via spontaneous vaginal delivery to a mom who had a history of marijuana use but stopped when she found out about her pregnancy. “There was no provider documentation indicating that the infant had any signs or symptoms of cannabis withdrawal; was affected by the maternal use of cannabis, nor any future healthcare implications for the baby.”
Because of the mom’s history, a urine drug screen was ordered for the infant. The results came back negative and the infant was discharged home.
Answer: Coding Clinic advised to code Z05.8 Observation and evaluation of newborn for other specified suspected condition ruled out, as a secondary diagnosis. Codes from category Z05 are used for newborns within the neonatal period, who are suspected to have an abnormal condition, but without signs or symptoms, and which after examination and observation, is found not to exist.
Hyperlipidemia v. Hypercholesterolemia:
Many think that hypercholesterolemia and hyperlipidemia are synonymous but they are not. Hypercholesterolemia is the medical term for high blood cholesterol level. It is a waxy substance produced by the liver and a component of all cells found in the body. Hyperlipidemia is when you have to many lipids or fats in your blood. Hypercholesterolemia is a type of hyperlipidemia.
Causes of hyperlipidemia:
1. Hereditary factors
2. Diet rich in saturated fats and cholesterol
3. Some diseases
4. Alcohol and smoking
5. Some medications
6. Steroids
Coding clinic recommends coding E78.00, Pure hypercholesterolemia, unspecified, for a diagnosis of unspecified hyperlipidemia and hypercholesterolemia. “Do not assign code E78.5, hyperlipidemia, unspecified, as the hypercholesterolemia identifies the specific blood lipid elevated.”1
Mixed hyperlipidemia means you have too much cholesterol and too much fat in your blood. Coding clinic recommends coding E78.2, Mixed hyperlipidemia, for a diagnosis of mixed hyperlipidemia with hypercholesterolemia and to not assign code E78.00, Pure hypercholesterolemia, unspecified, as the hypercholesterolemia is included in code E78.2.
1 AHA Second Quarter Coding Clinic 2022
Kidney Transplant:
Patients who have had kidney transplants may still have some form of Chronic Kidney Disease because the kidney transplant may not fully restore kidney function. Code Z94.0 Kidney transplant status may be assigned with a Chronic Kidney Disease code. “It is incorrect to assume that mild or moderate CKD following a transplant is a transplant failure unless it is documented as such in the medical record.”1
If there is documentation that a patient who has severe CKD or ESRD with a kidney transplant is having transplant failure or rejection or some other transplant complication code T86.1-, Complications of kidney transplant, is assigned. If the documentation is unclear whether there is transplant failure or rejection, it is necessary to query the provider because the CKD or ESRD alone is not a transplant complication.
Per Coding Clinic second quarter 2019 a patient with a history of a kidney transplant is admitted to the hospital with acute renal failure due to dehydration is assigned codes T86.19, Other complication of kidney transplant, N17.9, Acute kidney failure, unspecified, and E86.0, Dehydration, to capture the effect on the transplanted kidney with the ARF and dehydration. “Code T86.19 is assigned to capture the fact that the function of the transplanted kidney is affected by the ARF, but the transplant itself has not failed.”
1 AHA Handbook, Renal Disease, Diseases of the Genitourinary System
Anticoagulant:
Question: How is the diagnosis of long-term use of Eliquis coded in ICD-10-CM?
Answer: Coding Clinic advised to report Z79.01 Long- term (current) use of anticoagulants, for long term use of Eliquis.
Eliquis is classified as an anticoagulant medication. The drug Eliquis is used to prevent serious blood clots from forming due to a certain irregular heart beat (atrial fibrillation) or after hip or knee surgery.
Per Coding Clinic Second Quarter 2022 when a provider documents that a patient has a personal history of recurrent deep vein thrombosis of the lower extremity and is on anticoagulation therapy the following codes should be assigned Z86.718, Personal history of other venous thrombosis and embolism, and Z79.01, Long term (current) use of anticoagulants. This is coded for a patient that has no evidence of an acute, current or recurrent DVT nor complications from the thrombus. Chronic DVT is a thrombus that is one month to several months old and usually involves symptoms, such as chronic swelling, ulceration, cellulitis, or other complication. The provider would need to document recurrent or chronic DVT to code it as such.
Coding Clinic, Second Quarter 2020 & Coding Clinic, Second Quarter 2022.
Palliative Care:
Effective October 1,2021, code Z51.5 Encounter for palliative care, was added to the Exempt from POA Reporting List by the Centers for Disease Control and Prevention’s National Center for Health Statistics.
Effective April 1, 2022 the following diagnoses were designated as POA Exempt.
Z28.310 Unvaccinated for COVID-19
Z28.311 Partially vaccinated for COVID-19
Z28.39 Other under immunization status
To find a list of all diagnoses that are exempt from POA reporting go to the CMS.gov website.
https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/Coding
ICD-10-PCS Coding Tips
In this section:
- PCS Definitions
- Coronary Artery Bypass Grafts
- Coronary Intravascular Lithotripsy
- Impella

- Extraction of Bone Marrow from Other Sites
- Postop Drains
- Tubular Body Part Guideline Update
- Reconstructive Breast Surgery
- Tracheocutaneous Fistula
- Excisional and Non-excisional Debridement’s
- 53 New codes that were added to the New Technology Group for FY 2023
Disclaimer:
The information presented in this booklet is not intended to serve as coding or legal advice. Many variables affect code selection and sequencing. All coding must be considered on a case-by-case basis as supported by the documentation in the medical record. Payer-specific rules and regulations must also be taken into consideration in code selection. The information contained in this handout was accurate on the date of publication and is subject to change based on quarterly Coding Clinic updates from the American Hospital Association and yearly coding changes as determined by the National Center for Health Statistics and Centers for Medicare and Medicaid Services with approval from the World Health Organization.
PCS Definitions:
The ICD-10-PCS Official Guidelines for Coding and Reporting book begins with the following information:
“These guidelines are a set of rules that have been developed to accompany and complement the official conventions and instructions provided within the ICD-10-PCS itself. These instructions and conventions of the classification take precedence over guidelines.
…A joint effort between the healthcare provider and the coder is essential to achieve complete and accurate documentation, code assignment, and reporting diagnosis and procedures. These guidelines have been developed to assist both the healthcare provider and the coder in identifying those procedures that are to be reported. The importance of consistent, complete documentation in the medical record cannot be overemphasized. Without such documentation accurate coding cannot be achieved.”
Conventions for ICD-10-PCS
A. Conventions
A11.
Many of the terms used to construct PCS codes are defined within the system. It is the coder’s responsibility to determine what the documentation in the medical record equates to in the PCS definitions. The physician is not expected to use the terms used in PCS code descriptions, nor is the coder required to query the physician when the correlation between the documentation and the defined PCS terms is clear.
Example: When the physician documents “partial resection” the coder can independently correlate “partial resection” to the root operation Excision without querying the physician for clarification.
Coding Tip: For PCS-Coding, the proper code selection is driven by the provider’s documentation after is has been translated into PCS-terminology.
Coronary Artery Bypass of Coronary Arteries:
In coding Clinic Third Quarter 2021, a patient with coronary artery disease underwent a three-vessel aortocoronary bypass graft surgery. The patient underwent two reverse saphenous vein aortocoronary anastomoses, one from the ascending aorta to the right coronary artery (RCA) and one from the ascending aorta to the obtuse marginal (OM) artery. The left saphenous vein was harvested endoscopically. A left internal mammary artery (LIMA) free graft was also obtained and the distal end of the LIMA was anastomosed to the left anterior descending artery and the proximal end was anastomosed to the hood of the completed obtuse marginal saphenous vein graft.

Assign the following ICD-10-PCS codes:
021109W – Bypass coronary artery, two sites from aorta with autologous venous tissue, open approach, for the two coronary arteries bypassed from the aorta using the SVG
02100A3 – Bypass coronary artery, one artery from coronary artery with autologous arterial tissue, open approach, for the bypass utilizing a free LIMA graft between the obtuse marginal saphenous vein graft and the LAD. In this case, the obtuse marginal saphenous vein graft is functioning as a coronary artery. The LIMA graft allows blood flow from the functional coronary artery to the LAD. The ICD-10-PCS Official Guidelines for Coding and Reporting guideline B3.6a states that the qualifier value specifies the vessel bypassed from, therefore, qualifier “3, Coronary artery” is assigned (see green highlight on diagram above).
06BQ4ZZ – Excision of left greater saphenous vein, percutaneous endoscopic approach

*The reversed autologous SVG remains the preferable conduit for a coronary artery bypass. An SVG can function as a hood for a second graft as well. The indication for anastomosing a second vein or arterial graft onto a vein graft hood is an inadequate length of the second graft or the avoidance of proximal anastomosis on an atheromatous ascending aorta.
Coronary intravascular Lithotripsy:
Coronary intravascular lithotripsy (IVL) is a new treatment option for treating calcified lesions in the coronary arteries. Coronary IVL utilizes controlled sound waves in short pulses to selectively crack intimal and medial calcium within the vessel wall without affecting soft tissue. Once fractured, the calcium’s resistance to balloon dilatation is reduced, thereby allowing the blood vessel to be dilated using a low-pressure angioplasty balloon prior to coronary stenting. The coronary IVL catheter is advanced to the target lesion and the integrated balloon is inflated with fluid at a low pressure to contact the arterial wall. Coronary IVL is then activated, creating a small bubble within the catheter balloon that rapidly expands and collapses. The rapid expansion and collapse of the bubble creates sonic pressure waves that travel through the innermost layer of the vessel wall and crack the calcium within the vessel wall. Effective October 1, 2021 Table 02F was revised to include body part characters for coronary arteries.
**Coders should separately assign a separate applicable ICD-10-PCS code(s) for angioplasty or stent insertion if performed

Impella![]()
The intent of the Impella![]() system therapy is to reduce ventricular work and to provide the circulatory support necessary to allow heart recovery and early assessment of residual myocardial function.
system therapy is to reduce ventricular work and to provide the circulatory support necessary to allow heart recovery and early assessment of residual myocardial function.
It is a minimally invasive, catheter-based external cardiac assist device. The pump is inserted percutaneously into the left ventricle (through a peripheral artery). The Impella![]() device pumps blood for the left or right side of the heart into the ascending aorta or pulmonary artery. This is used to rest the patient’s heart during PCI (Percutaneous Coronary Intervention) procedures and prevents the heart from being overstressed while the coronary artery blockages are repaired. The device maintains blood flow and blood pressure during the procedure. The device is also used in patients with advanced heart failure and has the ability to improve the quality of life for these patients when there are no other options available.
device pumps blood for the left or right side of the heart into the ascending aorta or pulmonary artery. This is used to rest the patient’s heart during PCI (Percutaneous Coronary Intervention) procedures and prevents the heart from being overstressed while the coronary artery blockages are repaired. The device maintains blood flow and blood pressure during the procedure. The device is also used in patients with advanced heart failure and has the ability to improve the quality of life for these patients when there are no other options available.
In 2017 the qualifier “intraoperative” was added to 02H for insertion of short-term external heart assist system. Previously, guidance was to only code the assistance procedure (5A0) when the Impella![]() was inserted during the surgery only and removed. However, with the addition of this qualifier, coders are now to report both 02HA3RJ Insertion of short-term external heart assist system into heart, intraoperative, percutaneous approach and a code from (5A0221D) that describes continuous assistance with cardiac output using an Impella
was inserted during the surgery only and removed. However, with the addition of this qualifier, coders are now to report both 02HA3RJ Insertion of short-term external heart assist system into heart, intraoperative, percutaneous approach and a code from (5A0221D) that describes continuous assistance with cardiac output using an Impella![]() pump.
pump.
If the Impella![]() device is left in place for a few hours after surgery, the intraoperative qualifier would no longer apply since the device is still being utilized after patient has left the operating room. The ICD-10-PCS code for this situation would be reported as 02HA3RZ insertion of short-term external heart assist into heart, percutaneous approach and 5A0221D Assistance with cardiac output using Impeller pump, continuous.
device is left in place for a few hours after surgery, the intraoperative qualifier would no longer apply since the device is still being utilized after patient has left the operating room. The ICD-10-PCS code for this situation would be reported as 02HA3RZ insertion of short-term external heart assist into heart, percutaneous approach and 5A0221D Assistance with cardiac output using Impeller pump, continuous.
A “Duration” of intermittent setting on the Impella® device has been added along with “continuous” so coders must look at the medical record to ascertain if the duration was intermittent or continuous.
ICD-10-PCS New/Revised Codes — Section 0 – Medical & Surgical: Extraction of Bone Marrow from Other Sites:
In Table 07D, Extraction of Lymphatic and Hemic Systems, the body part value T Bone Marrow, has been added as shown below to identify when bone marrow is extracted from other sites, such as femur.

Per Coding Clinic for ICD-10-CM/PCS, Fourth Quarter 2021 – Drainage is the correct root operation when bone marrow is aspirated to obtain bone marrow cells suspended in fluid. Extraction is the root operation for removal of a sample of solid bone marrow.
Post Op Drains:
A common error found on both internal and external ICD-10-PCS audits is coding post-operative drains, such as a Penrose or Jackson Pratt drain (see Diagram below), as a drainage device. There is a PCS guideline B6.1b that specifically instructs us not to code temporary postop drains as drainage devices. This guidelines states “Materials such as sutures, ligatures, radiological markers and temporary post-operative wound drains are considered integral to the performance of a procedure and are not coded as devices.”
When coding procedures involving major surgery such as a sternotomy, joint replacements and organ removal or transplant post-operative drains are commonly placed to prevent fluid build-up and infections and are not coded. However, when the procedures involve incision and drainage of an abscess or other subcutaneous fluid and a postoperative drain is placed coders often assign a sixth character “0” for Drainage Device and this is incorrect. A sixth character of “Z” No Device should be assigned in these circumstances.

Tubular Body Part:
The ICD-10-PCS guideline B4.1c was updated to state that if a single procedure is performed on a continuous section of an arterial or venous body part, code the body part value corresponding to the anatomically most proximal (closest to the heart) portion of the arterial or venous body part. For example, a procedure performed on a continuous section of artery from the femoral artery to the external iliac artery with the point of entry at the femoral artery is coded to the external iliac body part. A procedure performed on a continuous section of artery from the femoral artery to the external iliac artery with the point of origin at the external iliac artery is also coded to the external iliac artery body part.1
1 2023 Official Coding Guidelines for Coding and Reporting
Reconstructive Breast Surgery:
Coding Clinic third Quarter 2022 describes a scenario in which a patient who is status post bilateral mastectomy and tissue expander placement presents for reconstructive surgery and removal of tissue expanders. The patient has a greater degree of capsular contracture with elevation of the tissue expander and breast contour on the left side than the right. “Prior to reconstructive surgery, bilateral partial capsulectomies were performed by excising and removing the anterior capsules along with the tissue expanders.” Coding Clinic advised based on the documentation submitted for this case to assign the following codes:
0HPT0NZ, Removal of tissue expander from right breast, open approach; and
0HPU0NZ, Removal of tissue expander from left breast, open approach, for the removal of the bilateral tissue expanders.
Note the partial capsulectomy procedures are considered inherent to the removal of the expanders and are not reported separately.
Per the documentation submitted to Coding Clinic both tissue expanders were removed with no mention in the documentation of any additional work or that a more complex removal was required.
Tracheocutaneous Fistula:
Coding Clinic First Quarter 2023 addresses the question of how to code the diagnosis for a patient that had undergone creation of a tracheostomy that was subsequently taken down in which the site remained open and currently has greenish discharge. Patient was admitted to the hospital to close the site. Coding clinic recommended to code the tracheocutaneous fistula following reversal to ICD-10-CM code J39.8, Other specified diseases of upper respiratory tract as the best available option. It was to discern that “the intent of the procedure (tracheostomy) is to create a fistula/stoma and failure of the stoma to close spontaneously is not classified as a ‘persistent postoperative fistula’ nor as a complication of the stoma.” Thus, code T81.83XA, Persistent postprocedural fistula, initial encounter, would not be appropriate.
Excisional & Non-excisional Debridement’s:

When an excisional debridement and a non-excisional debridement are performed at the same site but the non-excisional debridement is performed at a deeper layer which code(s) would be assigned?
Per Coding Clinic Second Quarter 2023, the fact the non-excisional debridement was performed at a deeper level does not affect code assignment. “When excisional and non-excisional debridement’s are both performed at the same site, report only the code for excisional debridement since this is the definitive procedure.”
53 New Codes Were Added to the New Technology Group for FY 2023:
Many of the new technology codes may be eligible for New technology Add-on Payment (NTAP). Below are just a few of the new codes.
- X0H – Insertion of Neurostimulator Lead into Sphenopalatine Ganglion, Vagus Nerve
- X0Z – Computer-assisted Transcranial Magnetic Stimulation of Prefrontal Cortex
- X2A – Intermittent coronary sinus occlusion
- XF5 – Destruction of liver using ultrasound-guided cavitation
- XKU – Supplement Upper Spine Bursa and Ligament with Posterior Vertebral Tether
- XNH – Insertion of Internal Fixation Device with Tulip Connector into Left or Right Pelvic Bone
- XRG – Fusion of Left or Right Sacroiliac Joint using Internal Fixation Device with Tulip Connector; Fusion using Interbody Fusion Device, Customizable
- XRH – Insertion of Posterior Spinal Motion Preservation Device into Lumbar and Lumbosacral Joints
- XRR – Replacement of lateral or medial meniscus with synthetic substitute
- XW0 – Introduction of Substance (several additions)
- XW1 – Transfusion of Substance into Central and Peripheral Vein
- XXE – Measurement of Coronary Artery Flow and Infection of whole blood; Measurement of Brain Electrical Activity with Computer-Aided Semiologic Analysis
- XY0 – Extracorporeal Antimicrobial Administration and Anticoagulant
Not coding new technology codes with NTAP is a frequent error that can cause hospitals thousands of dollars.